Keratoconus and astigmatism can cause blurred vision, glare, and night vision problems, affecting your visual clarity. Because they share symptoms, they’re often mixed up.
But while some symptoms of astigmatism and keratoconus overlap, others are distinct. Knowing the key differences can empower you to seek timely care and protect your sight.
Keep reading to learn more about how to know if your symptoms are keratoconus or astigmatism.
What is Astigmatism?

Astigmatism is a refractive error that occurs when the cornea, the clear dome-shaped layer at the front of the eye, has an irregular shape. In a normal eye, the cornea is evenly rounded like a baseball.
The smooth, round surface enables it to bend or refract incoming light so it focuses sharply on the retina, which is essential for clear vision. But with astigmatism, your cornea has an oval shape like a football.
This uneven shape prevents the cornea from bending light entering your eye correctly. As a result, the light doesn’t focus accurately on your retina, leading to distorted or blurred vision at all distances.
Astigmatism can occur alongside other refractive errors such as farsightedness and nearsightedness. It may worsen or improve over time.
Anyone can get astigmatism. Some people are born with it, while others develop it when they’re adults.
Applying too much pressure on your eyes or vigorous eye rubbing may also cause astigmatism.
What are the Symptoms of Astigmatism?
Astigmatism symptoms include:
- Blurred or distorted vision
- Headaches
- Eyestrain
- Halos and glare
- Eye fatigue
- Difficulty seeing at night
- Eye pain
- Squinting to try to see better
What is Keratoconus?
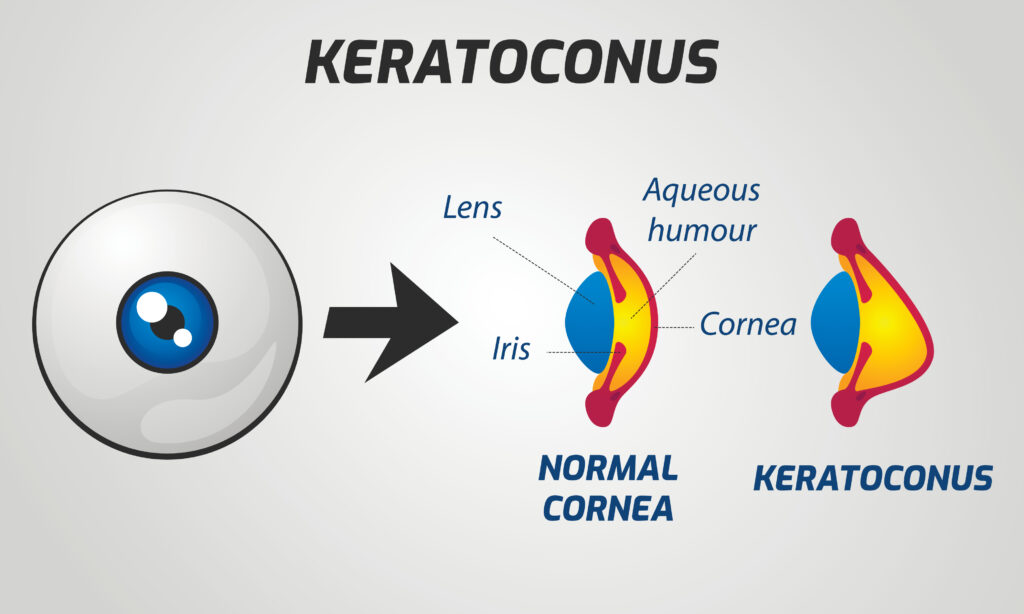
Keratoconus is a condition in which your cornea progressively thins and protrudes outward into a cone shape. The cone shape prevents incoming light from focusing as it should on your retina, causing your vision to become distorted.
Keratoconus typically develops in your teenage years and 20s. It can run in families.
It’s also linked to chronic eye rubbing, being African American or Latino, or inflammation from atopic eye disease, allergies, or asthma.
Additionally, studies have shown a connection between keratoconus and certain systemic conditions such as retinitis pigmentosa, Down Syndrome, Ehlers-Danlos syndrome, and osteogenesis imperfecta.
What are the Symptoms of Keratoconus?
Keratoconus symptoms may include:
- Blurred, distorted vision
- Eye discomfort
- Seeing halos
- Poor night vision
- Increased sensitivity to glare and light
- Double vision when looking out of one eye
- Progressively increasing astigmatism or nearsightedness
How Can You Tell If Your Symptoms Are Keratoconus or Astigmatism?
Both astigmatism and keratoconus affect the cornea. They also present similar symptoms, including blurred vision, halos, glare, and poor night vision.
That’s why they’re usually confused with each other. However, some symptoms are more commonly associated with keratoconus than with astigmatism.
If you experience double vision, sensitivity to light, and eye discomfort, you may have keratoconus. A cornea with keratoconus also has a cone shape, while an astigmatic cornea has an uneven curvature.
Needing to change your prescription frequently due to worsening astigmatism or nearsightedness is another tell-tale sign of keratoconus. Unlike astigmatism, prescription eyeglasses might not fully correct distorted or blurry vision as keratoconus progresses.
Keratoconus causes severe vision distortion over time and may require more specialized treatment, such as specialty contact lenses or surgical intervention in more advanced cases.
How are Keratoconus and Astigmatism Diagnosed?
If you’re experiencing changes in your vision, the first step should be to consult your eye doctor at Cheema MD Eye Care. That’s the only way to know for sure if you have keratoconus or astigmatism.
They’ll perform a comprehensive eye exam and several tests to determine the cause of your symptoms, including a corneal topography scan. This scan checks for distortions and imperfections on the corneal surface to help differentiate the symptoms of keratoconus and astigmatism.
Your eye doctor may also perform a keratometry. The test evaluates your corneal curvature and can determine the severity of your astigmatism.
Diagnosing astigmatism may also involve using an eye chart to test visual acuity at various distances. In addition, your eye doctor may do a refraction test to measure how well your cornea focuses light on the retina.
How are Keratoconus and Astigmatism Treated?

Astigmatism can be corrected with prescription glasses or contacts. For patients seeking freedom from visual aids, vision surgery options such as LASIK, PRK, SMILE, EVO ICL, or RLE can significantly reduce or even eliminate the need for corrective lenses.
Keratoconus treatment depends on the severity of the condition. In the early stages, soft contact lenses or eyeglasses can help correct mild vision changes.
However, as the condition progresses, glasses and soft contacts may not adequately correct your eyesight. When this happens, your ophthalmologist may prescribe rigid gas-permeable, piggyback, hybrid, or scleral contact lenses to improve your vision by forming a smooth surface over your cornea, allowing light to focus accurately on your retina.
If keratoconus gets worse, corneal cross-linking can be the next line of treatment. For this procedure, your ophthalmologist will saturate your cornea with riboflavin eyedrops and treat it with ultraviolet light.
This will stabilize and strengthen the corneal structure, which can slow or even halt the progression of keratoconus. Corneal cross-linking can also reduce the cone shape of the cornea, enabling you to see better with contact lenses.
As keratoconus progresses, your ophthalmologist may suggest Intacs. Intacs are a pair of transparent, crescent-shaped implants that are placed into your cornea to flatten it.
They make it easier to wear contact lenses again. In some cases, a corneal transplant may be necessary if your keratoconus is too advanced for other treatments to work effectively.
It involves replacing the damaged cornea with a healthy donor cornea. Even after the procedure, you’ll likely continue needing glasses or contact lenses to see clearly.
Don’t Let Keratoconus or Astigmatism Limit Your Vision
It’s crucial to see your ophthalmologist as soon as you notice any vision changes. Dr. Cheema has extensive experience treating corneal conditions and utilizes cutting-edge diagnostic and treatment capabilities to effectively manage keratoconus and astigmatism.
Do you suspect you have keratoconus or astigmatism? Schedule your appointment at Cheema MD Eye Care today for prompt, accurate diagnosis and best-in-class treatment to safeguard your sight.